By Lindsay Wiliams, PhD
If you’ve been watching the news lately, you’ve likely heard about a “tripledemic” that is starting to affect our country. Indeed, many medical experts are advising us about a potential three-way winter virus surge: COVID-19, flu and RSV (officially known as respiratory syncytial virus).
We’re all used to higher levels of sickness going into winter; in fact, two of the biggest COVID-19 spikes centered around January in both 2021 and 2022. However, unlike the last two winters, most of the United States now operates largely without dedicated health mitigation measures. This could make Americans more vulnerable to catching any disease as the temperature drops.
Our best hope to tackle a winter virus surge head-on is to know what to expect from it — and which tools are at our disposal. So, I’ve answered some general questions about the emerging tripledemic to help you feel prepared.
Why do winter virus surges happen?
Respiratory diseases have always demonstrated higher rates of spread during the winter — long before COVID-19 entered the picture.
Of course, social changes during winter months can result in higher rates of infection. We tend to hold far more indoor gatherings, huddling close together in poorly ventilated spaces. Less time outdoors also means less time in the sun and lower vitamin D levels, leading to weakened immune systems.
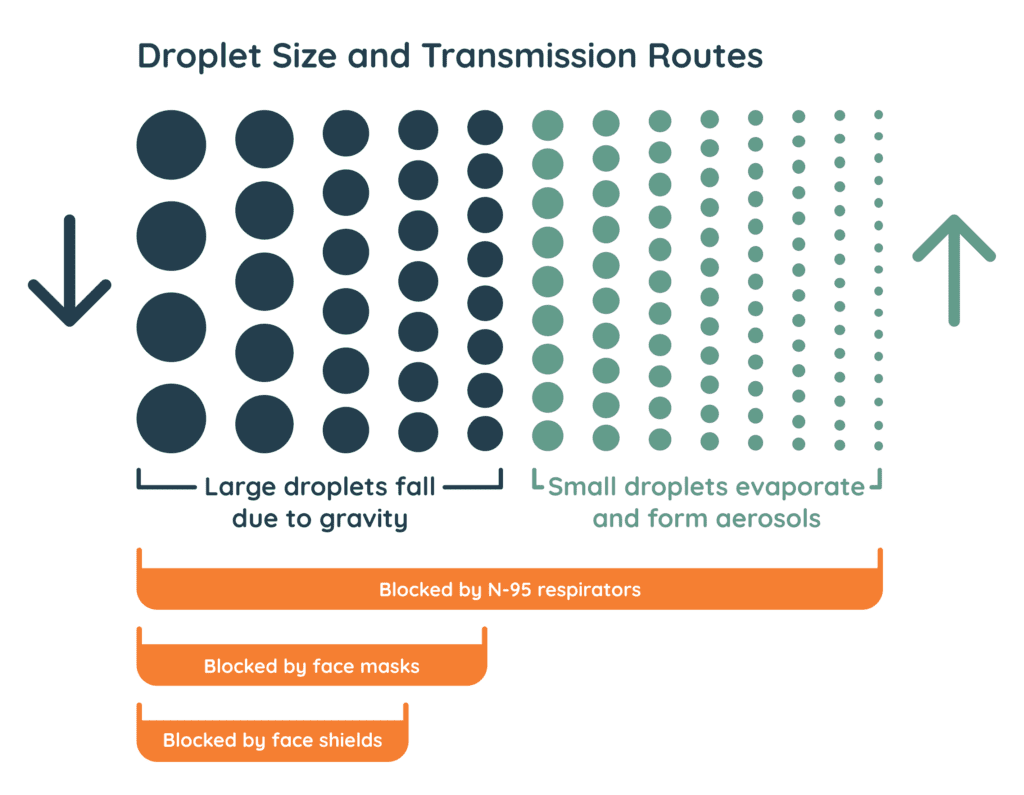
The weather itself plays a role too — but not so much the temperature as the change in humidity. Disease-carrying respiratory droplets take on more moisture and fall to the ground more quickly when it’s humid out. Take that humidity away and these droplets hover in the air for longer, making them more likely to infect someone.
Again, this is nothing new: Respiratory diseases like the flu have always spiked this time of year. Still, you shouldn’t let your guard down, especially in a potentially challenging winter like this one.
How might this winter be different from previous ones?
The pandemic brought flu spread to record lows in previous winters, largely thanks to COVID-19-related health mitigation measures.
Most of us stayed socially distant around the 2020 and 2021 holidays and wore masks in public. So, the flu simply didn’t have much opportunity to spread from person to person. (The generally more-contagious COVID-19, of course, raged during those periods.)
But now that mask mandates and other mitigation measures have been mostly lifted, we’ve reopened many avenues for any virus to spread. New cases of both flu and RSV already have increased disproportionately this year.
On top of these comebacks, new subvariants of the omicron coronavirus strain have emerged, called “Scrabble variants” by some. Two in particular, BQ.1 and BQ.1.1, are spreading at an alarming rate; the second is notorious for its ability to evade COVID-19 immunity from vaccination or prior infection.
What can I do about it?
My advice for people trying to stay safe during COVID-19 has been the same since the pandemic began. Still, it bears repeating.
First, get up to date on all necessary vaccinations and boosters. While new COVID-19 subvariants like BQ.1.1 can “cut through our immunity” better than previous ones, they’re still descendants of the omicron variant. Therefore, omicron boosters remain the best way to develop antibodies that’ll help protect you from serious illness or hospitalization. Likewise, getting a flu vaccine will help protect you from severe cases of influenza. And while no RSV vaccine is yet available, scientists are hoping to get one approved by the Food and Drug Administration this year.
Second, get used to the idea of readopting health mitigation measures. I know — wearing a mask, maintaining 6 feet of distance from others and abstaining from large gatherings aren’t anyone’s idea of fun. But as respiratory droplets linger in the air for longer, these are some of the best ways to avoid exposure. Even if these strategies aren’t mandatory where you live or you’re the only one in your social circle who observes them, your top priority should be protecting yourself and your loved ones. And as we’ve seen in the past couple of years, health mitigation strategies don’t just help you avoid COVID-19, but also the flu and other respiratory infections.
Third (and perhaps most importantly), get tested regularly. Symptoms can only tell you so much about your current health status. Symptoms for COVID-19, the flu, RSV, allergies and the common cold often overlap. Testing is the best way to know where you stand healthwise.
Different kinds of COVID-19 tests are better for different scenarios. Antigen tests yield results in just a few minutes. They’re generally the less accurate option but tend to be very reliable if you’re showing symptoms. PCR tests take longer but can detect early infection with high accuracy; they’re best for peace-of-mind testing or before you socialize with others. This makes PCR the ideal option before you visit older or otherwise immunocompromised family for the holidays.
(Our PCR tests yield results in 24 hours or less, guaranteed. Click here to see if we offer them in your area.)
If you or a loved one feels ill but tests negative repeatedly for COVID-19, you or they could still have a serious disease. Visit your personal care provider or a nearby urgent care clinic to get tested for other respiratory infections. Some providers (including select Worksite Labs locations) also offer “triplex” testing, in which patients are tested for influenza A, influenza B and COVID-19 all at once. This is a great option for anyone who doesn’t know what they’re sick with and wants to begin recovery ASAP.
Finally, if you test positive for COVID-19 at home, report the results to your personal care provider and local public health department. This will help you kick-start your recovery the right way — your provider can prescribe the right treatment for you and will give your local government the necessary data to assess the current health situation.
What should local and state governments do about it?
The pandemic demonstrated that a near-overnight outbreak of a serious contagion can force society to hit the brakes. So, our elected leaders should act accordingly this winter.
The best thing local and state governments can do is listen to researchers, scientists and other experts. They can often forecast disease spread months in advance based on epidemiological data from around the world. For instance, experts roughly predicted when the coronavirus “Scrabble variants” might pop up in the United States based on their emergence in other parts of the Northern Hemisphere. They also pinpointed an unexpected rush of RSV in the summer of 2021 as businesses reopened and Americans started shedding their masks.
Based on professional research and recommendations, our leaders should regularly evaluate whether mandates are necessary to slow disease spread. One useful method is to implement tiered thresholds of community mitigation. By adjusting health mandates based on the current level of community transmission, localities can keep businesses and schools operating as fully as possible while also curbing disease spread.
That’s why it’s so important to frequently report data on local transmission. Health departments should consider reporting new cases daily during notable surges so that the communities they serve can respond in kind.
How can our country better prepare for future spikes in disease?
From a healthcare and clinical standpoint, building a decentralized lab testing network is the best solution to handle an overwhelming need for quality care in our country.
Diagnostic testing is a key component to protecting people during virus surges. But when testing demand increases, the U.S. lab system slows down significantly, with millions of tests getting funneled into a handful of centralized, regional testing labs.
Conversely, placing decentralized labs near healthcare providers and other organizations dramatically reduces turnaround times for test results, even during periods of high transmission. This is due to the reduced travel time between the collection site and processing lab, as well as the ability of decentralized labs to flex their capabilities to meet ever-changing needs.
By transitioning U.S. testing to a decentralized model, we could revolutionize our national response to future spikes in disease spread.
Contact us if you’re interested in bringing decentralized lab testing to your area.
Lindsay Williams, PhD, is chief nursing officer of Worksite Labs.