You’ve probably had your share of conversations about COVID-19 over the last two years. And I’ll bet in at least one of those, you or someone else said something like: “Well, as soon as the coronavirus becomes endemic, things will be OK again.”
But what might endemic COVID-19 look like? And what does the word endemic even mean?
Let’s walk through the differences between endemic diseases and other outbreaks, what we can expect from the endemic phase of COVID-19 and when we might reach it.
What’s the difference between an endemic disease, and and an epidemic?
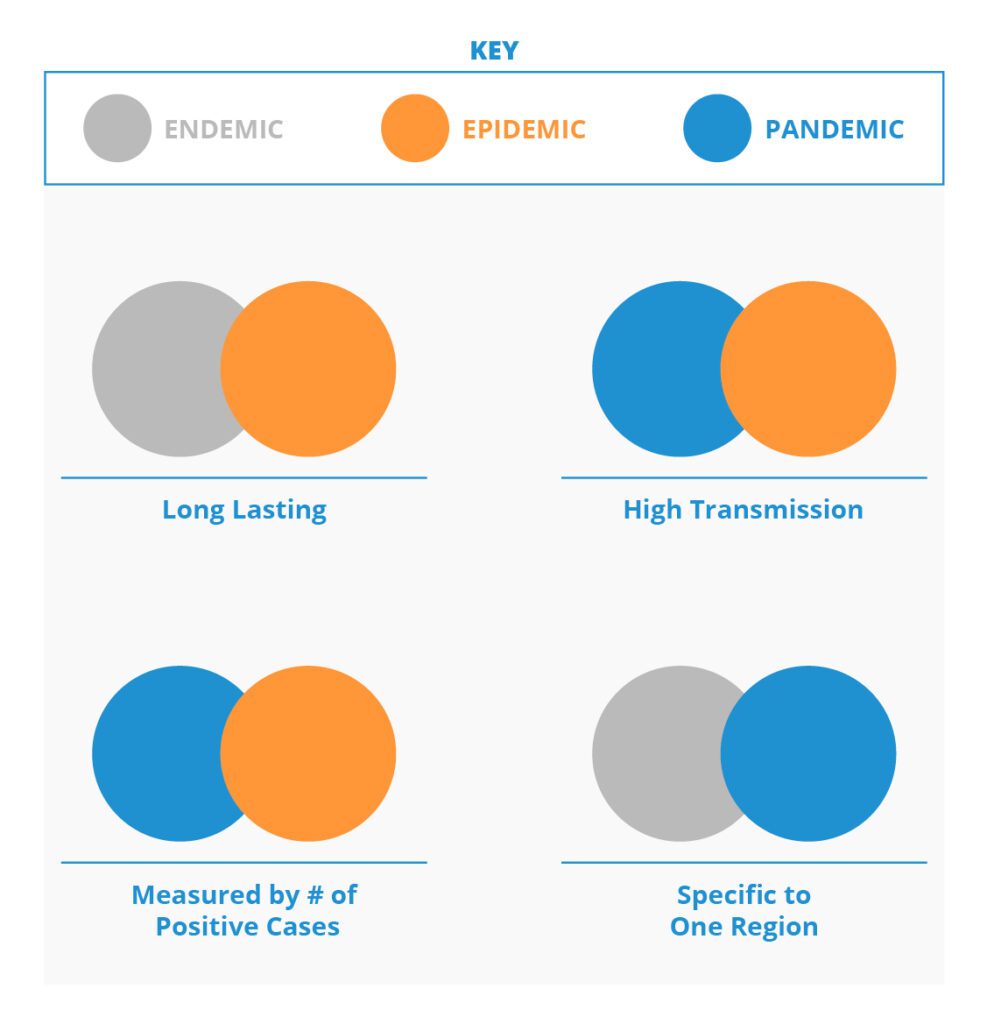
Health authorities define endemic diseases by their severity, while pandemics and epidemics are defined by where outbreaks occur and the volume of cases.
A disease is endemic when it’s constantly “in the background” and stays at a steady, relatively low transmission level.
People aren’t suffering severe illness, landing in the hospital or upending their daily life as schools and businesses close their doors. Authorities track the hospitalization rates to measure an endemic disease’s spread, rather than simply the case count.
An epidemic is a large outbreak of an infection in a particular region or area in a relatively short timeframe.
An example you might remember is the Western African Ebola virus outbreak of 2014-16. (It technically spread overseas, but it’s still called an epidemic because it remained majorly concentrated in one region.)
A pandemic occurs when an infection spreads across multiple countries and continents, affecting a large chunk of the population.
Authorities evaluate its spread based on positive case count. Before it became endemic, the influenza pandemic spread worldwide and killed tens of millions in the early 20th century.
Epidemics (or outbreaks) can occur during an endemic disease when an area or population sees a notable spike in cases. And experts say it’s possible to move back and forth from pandemic to epidemic phases; once COVID-19 reaches endemic status, it won’t necessarily be permanent.
Are we approaching the endemic phase of COVID-19?
Yes. White House Chief Medical Adviser Dr. Anthony Fauci said in April that we’re out of the “acute component of the pandemic phase” and transitioning “to more of an endemicity,” and I agree.
The omicron variant was a major turning point since it was highly contagious but not very lethal. By infecting millions of people with many different mutations of SARS-CoV-2, it helped our country build a whole library of antibodies against future spread.
That natural immunity, combined with vaccine immunity, helps lower the overall severity of COVID-19 and moves us toward that endemic stage. Keep in mind, we know for sure that vaccine and natural immunity wane over time, evidenced by people being reinfected regardless of vaccine status. The best way to ensure our country’s collective antibody count stays high is to continue vaccine programs and development and hope the variants remain mild so even more antibodies can be produced via natural immunity.
Now that we have an immune response to the virus, it’s basically becoming another version of the common cold. That’s the hope, at least.
Is there a line in the sand that determines when exactly COVID-19 becomes endemic?
No. Endemic has no fixed, empirical definition. COVID-19 won’t simply be declared endemic once it sinks to a certain number of cases or hospitalizations per 100,000 people.
Health officials will have to determine whether the virus has become relatively stable and manageable without disruptive measures in place. Until then, COVID-19 is still a pandemic.
How will public behavior change when COVID-19 reaches endemic status? How should I change my own behavior?
We’ve already seen the beginnings of changing public behavior as endemic COVID-19 approaches.
Masks aren’t required on public transportation or airplanes anymore as of late April. Most U.S. states don’t require them at schools or in public settings. In-person work has largely resumed for many companies and industries that previously went remote or hybrid. As we near endemic COVID-19, similar back-to-normal changes are bound to continue.
“You’re responsible to keep your and others’ safety in mind, even if it feels ‘overly cautious’ at times.”
But what’s required and what’s right don’t always overlap.
You’re responsible to keep your and others’ safety in mind, even if it feels “overly cautious” at times. Mask up in group settings if you’re not feeling well or were recently exposed to COVID-19. And even if you feel 110%, maintain proper hygiene and wash your hands frequently.
You’d stay home from work or school if you were exposed to the flu or a common cold, right? Similarly, act in a way that protects others from endemic COVID-19.
What role will diagnostic testing play during endemic COVID-19?
Endemic diseases aren’t harmless, and endemic COVID-19 won’t be any different. As long as the coronavirus poses a health threat, testing will remain the most consistently effective safeguard against its spread.
Testing during the endemic stage will help you:
- Protect immunocompromised friends and family when you visit them.
- Keep your school or workplace safe in periods of higher transmission or epidemics.
- Access test-to-treat services (like those offered at our downtown San Francisco site) if you become infected.
Endemicity will inevitably change many things about how we respond to the coronavirus. The power of testing won’t be one of them.
Christopher Reeves, MD, is chief medical officer of Worksite Labs.